Urinary Incontinence: Causes, Types, and Treatment Methods
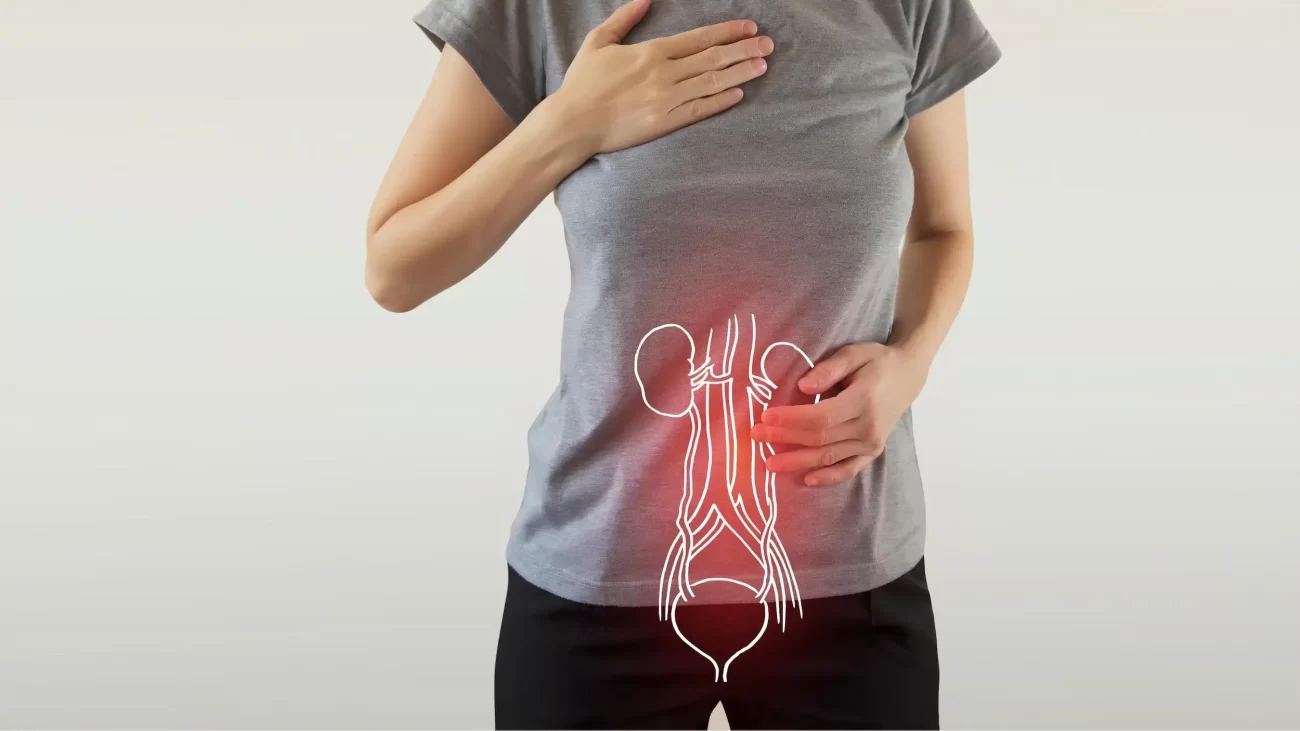
Urinary incontinence is the involuntary loss of urine, a common health issue that negatively affects the quality of life for both men and women. Urinary incontinence can arise from various causes and manifest in different ways. Fortunately, modern treatment methods today allow for effective management of urinary incontinence.
What is Urinary Incontinence?
Urinary incontinence is the involuntary leakage of urine due to the inability to control bladder function. This condition can range from minor leaks to complete bladder emptying. While urinary incontinence is often seen as a natural consequence of aging, it can also occur in younger individuals for various reasons. If left untreated, it can adversely impact a person’s social life, self-esteem, and overall health.
Types of Urinary Incontinence
There are several different types of urinary incontinence, each arising from distinct causes:
- Stress Incontinence: This type occurs when there is an involuntary leakage of urine during moments of increased abdominal pressure, such as coughing, sneezing, laughing, or heavy lifting. It usually results from weakened pelvic floor muscles or insufficient support of the bladder neck. Major causes in women include pregnancy, childbirth, and menopause.
- Urge Incontinence: This type begins with a sudden and strong urge to urinate, which the person cannot control, leading to involuntary leakage. This condition is often due to involuntary contractions of the bladder muscles, known as overactive bladder. Causes can include nerve damage, urinary tract infections, or neurological diseases (such as Parkinson’s disease or multiple sclerosis).
- Overflow Incontinence: This occurs when the bladder cannot be completely emptied, causing urine to leak out in small amounts. The bladder remains full but cannot void, leading to overflow. This type is typically caused by weak bladder muscles, bladder obstructions, or neurological disorders.
- Mixed Incontinence: This type includes symptoms of both stress and urge incontinence. It is commonly seen in women and incorporates symptoms from both types.
- Functional Incontinence: This type arises from physical or cognitive impairments that prevent a person from reaching the toilet in time. Conditions like arthritis that restrict mobility or cognitive disorders like dementia can lead to this type of incontinence.
Causes of Urinary Incontinence
Urinary incontinence can stem from multiple factors. These causes can vary based on age, gender, lifestyle, health conditions, and genetic factors. The primary causes of urinary incontinence include:
- Weakness of Pelvic Floor Muscles: These muscles support the bladder and urethra. Weakness in these muscles can lead to inadequate bladder control. Conditions such as childbirth, pregnancy, obesity, and menopause can weaken these muscles.
- Hormonal Changes: In women, decreased estrogen levels after menopause can weaken the bladder and urinary tract tissues, increasing the risk of urinary incontinence.
- Prostate Issues: In men, an enlarged prostate can narrow the urethra, preventing complete bladder emptying, which can lead to overflow incontinence. Additionally, urinary incontinence may occur after prostate surgery.
- Neurological Disorders: Conditions like Parkinson’s disease, multiple sclerosis, stroke, and spinal cord injuries can affect bladder control and cause urinary incontinence.
- Urinary Tract Infections: These infections can irritate the bladder and cause it to become overactive, leading to urge incontinence.
- Aging: As one ages, bladder muscles weaken, and bladder capacity decreases. Control of bladder muscles also becomes more difficult, increasing the risk of urinary incontinence.
- Obesity: Excess weight increases pressure in the abdominal area, putting extra strain on the bladder, particularly leading to stress incontinence.
Diagnosis of Urinary Incontinence
When individuals experiencing urinary incontinence consult a specialist, a detailed evaluation process begins. The doctor reviews the patient’s medical history and conducts a physical examination, potentially ordering some of the following tests:
- Urinalysis: Conducted to identify urinary tract infections or other abnormalities.
- Ultrasound: Used to visualize the bladder and kidneys.
- Cystoscopy: An examination using a camera to inspect the inside of the bladder.
- Urodynamic Testing: Tests that evaluate bladder function and pressure levels.
Treatment Methods for Urinary Incontinence
Treatment for urinary incontinence varies based on the type, severity, and underlying causes of the issue. Treatment options range from lifestyle changes to surgical interventions.
- Lifestyle Changes:
- Regulating Fluid Intake: Balancing fluid intake throughout the day can reduce nighttime urination frequency.
- Limiting Caffeine and Alcohol: These substances can irritate the bladder and increase urine production.
- Regular Weight Loss: Being overweight can increase the risk of urinary incontinence, so losing weight may alleviate symptoms.
- Quitting Smoking: Smoking can lead to chronic cough and weaken pelvic floor muscles.
- Pelvic Floor Exercises (Kegel Exercises): These exercises strengthen the pelvic floor muscles and can be very effective in managing stress incontinence. They help regain muscle control and, when performed regularly, can reduce incontinence.
- Bladder Training: This method involves retraining the bladder to control urination frequency. Bladder training teaches the bladder to hold urine for longer periods and is typically used to treat urge incontinence.
- Medication: In some cases, medication may be prescribed to relax bladder muscles or strengthen pelvic floor muscles. For instance, medications used for overactive bladder can reduce urge incontinence.
- Electrical Stimulation: This method uses low-voltage electrical impulses to strengthen pelvic floor muscles and improve bladder control.
- Surgical Options: Surgical intervention may be necessary in more severe cases of urinary incontinence. Surgical methods vary based on the type of incontinence:
- Sling Surgery: A sling is placed to support the urethra in cases of stress incontinence.
- Bladder Neck Suspension: Surgery to provide better support for the bladder neck.
- Artificial Sphincter Placement: An artificial sphincter can be placed if the natural sphincter muscle is not functioning properly.
Urinary incontinence, while a challenging issue that can negatively impact quality of life, has many effective treatment options available today. The appropriate treatment based on the source of the problem can help alleviate symptoms and enable individuals to return to their normal lives. If you are experiencing urinary incontinence, it is advisable to consult a specialist to learn about suitable treatment options for you.
